


PRENATAL DIAGNOSIS OF TRANSLOCATION 13;13
PATAU SYNDROME: CLINICAL FEATURES OF TWO CASES
Pazarbaþi A1,*, Demirhan O1, Süleymanova-Karahan D1,Taþtemir D1,
Tunç E1, Gümürdülü D2
*Corresponding Author: Ayfer Pazarbaþi, Ph.D., Department of Medical Biology and Genetics,
School of Medicine, Çukurova University, 01330 Balcali, Adana, Turkey; Tel.: +90-322-338-70-
68; Fax: +90-322-338-65-72; E-mail: payfer@cu.edu.tr
page: 69
|
|
INTRODUCTION
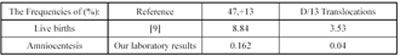
Changes in number or structure of chromosomes are a major cause of congenital anomalies and intellectual impairment. Trisomy 18 is the second and Trisomy 13 the third most common autosomal trisomy at birth [1,2]. Non disjunction is the failure of one or more pairs of homologous chromosomes to separate following the first or second meiotic division. Trisomy 13 usually involves a maternal meiotic error but paternal errors also occur [3]. When reduction (separation pairs of homologous chromosomes) does not occur, non disjunction occurs and is responsible for autosomal trisomies. Studies suggest a common mechanism for occurrence with all trisomies [2,4]: maternal first meiotic division (40% of cases); maternal second meiotic division (40% of cases); paternal first meiotic division (20% of cases) About 80% of trisomy 13 cases result from fresh mutations, and the remainder occur as a result of chromosomal translocation. During translocation, chromosomes misalign and join at their centromeric region with subsequent loss of part of a chromosome. This is called a Robertsonian translocation. During Robertsonian translocation, the long arms of two acrocentric chromosomes fuse at the centro mere and the two short arms are lost. Common Robert sonian translocations are confined to acrocentric chromosomes 13, 14, 15, 21, and 22, as the short arms do not contain essential genetic material. Chromosome 13:14 Robertsonian translocations account for up to 33% of all Robertsonian translocations. Parents may have children with a normal number of chromosomes, a trisomy, a monosomy, or a balanced translocation [1]. Robertsonian translocations are the most common human structural chromosomal abnormalities with an incidence of 1.23/ 1000 live births [5,6]. They are mainly observed in group D chromosomes (i.e., 13, 14, 15) and group G (i.e., 21 and 22). The D/D translocation is the most frequent type, with a high predominance of 13;14 translocations [6,7]. In Robertsonian translocations, the pericentric regions of two acrocentric chromosomes fuse to form a single or two centromeres. The resulting balanced karyotype has only 45 chromosomes including the translocated one, which is a result of a fusion of the long arms of two chromosomes. Malsegration (unbalanced segration) of Robertsonian translocation, results in trisomy or monosomy of complete chromosomes [8]. Patau syndrome is associated with extra chromosome 13 material, either free as in the 47,+13 genotype or in a Robertsonian translocation or another rearrangement. This genotype occurs in: 1) about 0.8-1.0% of spontaneous abortuses; 2) about 0.4% of early neonatal deaths; and 3) amniocentesis, higher than in live births, at least for mothers 40 years and over [9]. Trisomy 13 occurs in about 1 out of 10,000 live and still births. However, the actual prevalence of trisomy 13 is difficult to estimate because many pregnancies involving a prenatal diagnosis of trisomy 13 are terminated shortly after the diagnosis has been made [10]. The frequencies of 47,+13 was 0.162% and the frequencies of D/13 translocations was 0.04% according to our laboratory results of 4,300 prenatal diagnoses with amniocentesis (unpublished data). The results of Hook et al. [9] in a total of 113,045 studied live births and our laboratory are shown at Table 1. In this study we report the clinical features, genetic (cytogenetic screening for all chromosomal disabilities) and autopsy findings of two trisomy13 cases.
Table 1. The frequencies in amniocentesis and in live births
|
|
|
|



 |
Number 27
VOL. 27 (2), 2024 |
Number 27
VOL. 27 (1), 2024 |
Number 26
Number 26 VOL. 26(2), 2023 All in one |
Number 26
VOL. 26(2), 2023 |
Number 26
VOL. 26, 2023 Supplement |
Number 26
VOL. 26(1), 2023 |
Number 25
VOL. 25(2), 2022 |
Number 25
VOL. 25 (1), 2022 |
Number 24
VOL. 24(2), 2021 |
Number 24
VOL. 24(1), 2021 |
Number 23
VOL. 23(2), 2020 |
Number 22
VOL. 22(2), 2019 |
Number 22
VOL. 22(1), 2019 |
Number 22
VOL. 22, 2019 Supplement |
Number 21
VOL. 21(2), 2018 |
Number 21
VOL. 21 (1), 2018 |
Number 21
VOL. 21, 2018 Supplement |
Number 20
VOL. 20 (2), 2017 |
Number 20
VOL. 20 (1), 2017 |
Number 19
VOL. 19 (2), 2016 |
Number 19
VOL. 19 (1), 2016 |
Number 18
VOL. 18 (2), 2015 |
Number 18
VOL. 18 (1), 2015 |
Number 17
VOL. 17 (2), 2014 |
Number 17
VOL. 17 (1), 2014 |
Number 16
VOL. 16 (2), 2013 |
Number 16
VOL. 16 (1), 2013 |
Number 15
VOL. 15 (2), 2012 |
Number 15
VOL. 15, 2012 Supplement |
Number 15
Vol. 15 (1), 2012 |
Number 14
14 - Vol. 14 (2), 2011 |
Number 14
The 9th Balkan Congress of Medical Genetics |
Number 14
14 - Vol. 14 (1), 2011 |
Number 13
Vol. 13 (2), 2010 |
Number 13
Vol.13 (1), 2010 |
Number 12
Vol.12 (2), 2009 |
Number 12
Vol.12 (1), 2009 |
Number 11
Vol.11 (2),2008 |
Number 11
Vol.11 (1),2008 |
Number 10
Vol.10 (2), 2007 |
Number 10
10 (1),2007 |
Number 9
1&2, 2006 |
Number 9
3&4, 2006 |
Number 8
1&2, 2005 |
Number 8
3&4, 2004 |
Number 7
1&2, 2004 |
Number 6
3&4, 2003 |
Number 6
1&2, 2003 |
Number 5
3&4, 2002 |
Number 5
1&2, 2002 |
Number 4
Vol.3 (4), 2000 |
Number 4
Vol.2 (4), 1999 |
Number 4
Vol.1 (4), 1998 |
Number 4
3&4, 2001 |
Number 4
1&2, 2001 |
Number 3
Vol.3 (3), 2000 |
Number 3
Vol.2 (3), 1999 |
Number 3
Vol.1 (3), 1998 |
Number 2
Vol.3(2), 2000 |
Number 2
Vol.1 (2), 1998 |
Number 2
Vol.2 (2), 1999 |
Number 1
Vol.3 (1), 2000 |
Number 1
Vol.2 (1), 1999 |
Number 1
Vol.1 (1), 1998 |
|
|

